I know myself just how draining that is. And lifestyle change seemed so daunting. I mean the very phrase insinuates huge change.
But then one little change fixed everything.Instead of trying to fix my diet, or change my habits overnight, I decided to fix my mindset.
But I didn’t, and still don’t use any willpower to maintain this at all.
And to be honest… it wasn’t really that hard at all.

I’m not trying to sell you shit.
So what did I do?
1) I told myself it would take time.
2) I let myself be human, and cheat or fail every now n then. Well, regularly, to be honest.
3) I took a step back and changed how I looked at food.
4) I challenged the thought processes that made me keep wanting to eat, while I was eating. I challenged these regularly. I rewarded myself regularly with congratulations and self-applause when I made the right choice. If I couldn’t help it, I’d make an excuse, knowing that I was forming neural networks that would solidify in the long run.
5) I SLOWLY – we’re talking 1 pizza slice less per month – reduced my portion sizes.
6) I ATE WHATEVER I WANTED – and let myself be human, knowing, that by reducing my portion sizes slowly over time, my stomach would get smaller and my brain would form neural pathways would make NEW thought processes that would become my habit.
The most important part of this process is STEP NUMBER 3! Repeating step 3 for JUST THREE WEEKS HAS MEANT…
7) I didn’t have to do anything else. I don’t have to do anything else. Ever. Neuoroplasticity has ensured that I never
have to try to diet or lose weight, EVER.
That’s it.
But keep reading to understand WHY step 3 is important, and how you can and should be doing this.
Check out my 40 page book which summarises all of this and cites everything
I hope it can help. And email me if you ever wanna talk. Keep reading on and I hope this helps.
Everyone talks about how they can’t stay on a diet and how they can’t find the time to do exercise… They talk about how hard it is to make changes in their life and how they just don’t have the willpower or ability to be healthier people.
But even while on 50mg of prednisone, a corticosteroid (which increases your appetite, screw around with your hormones and energy metabolism, and eat away at muscles) and even while I was still getting some chemotherapy which makes me anaemic for a one or two weeks every month, I didn’t find it hard at all.
All I did to become a healthier person was change my MINDSET.
I made healthy habits and eating less – a habit. The path of least resistance.
Automatic. And you can too.
Doctors all tell us that weight loss requires a lifestyle change, rather than drastic, quick-fix 12-day-detox/Biggest Loser boot camp solutions. And they’re right. You should look to lose weight AND keep it off. It’ll help you with heart problems, lower your chances of diabetes, reduces your risk of cancer and also – a healthy diet can make you feel better, more energetic than ever before.
But the words “lifestyle change” imply that it’s hard, that it requires constant effort and struggle to do, and that’s a big reason why people aren’t willing to make that change.
Eating the right foods, and getting some exercise on a continuous basis IS vital to weight loss. But what’s even more important is if you can maintain that way of living.
In hthis picture, I was sitting at around 106-107kg. I was trying everything to get fit and lose weight. I started juicing, cutting carbs out of my diet and went out, trying to run, get back into my old sprint training and back into the weights. And that was working – as it would for anyone – for a few weeks at a time.

Before: 107kg
But with my low immunity putting me into hospital with infections every few months, with my treatments lowering my bloodcounts, I kept getting sent back to where I began from over and over again… and it was frustrating as hell.
I yoyo dieted. Like crazy. I calorie counted. Stopped carbs. Intermittent fasted. Got into calorie deficits.
But dieting is hard. Forcing yourself to not eat is unnatural and really hard to do consistently.
I wanted to lose weight and become as fit as I was before cancer… I wanted to see results… but they just weren’t coming.
But after a while of this, I took a step back and saw that I was going through a cycle over and over again. It’s the same cycle a lot of yoyo/fad dieters go through.
I wanted results and I wanted them NOW. But they weren’t coming.
You don’t need huge “willpower” to do it. All it takes are a few small changes in how you view things.

But I’d lost nearly 20kg. It looks like a lot, but really, it was 1kg/week.
The only time I gained weight again after that first burst of weight loss was 5 years ago, when I got a third cancer in my ribs, was in hospital, and when I thought I’d need chemo again. I got back to my normal weight 6 months after that. Without trying.
So how exactly did I get there?
And how can you do this too?
1) I told myself it would take time.
2) I took a step back and changed how I looked at food.
3) I challenged the thought processes that made me keep wanting to eat, while I was eating. I challenged these regularly. I rewarded myself regularly with congratulations and self-applause when I made the right choice. If I couldn’t help it, I’d make an excuse, knowing that I was forming neural networks that would solidify in the long run.
4) I SLOWLY – we’re talking 1 pizza slice less per month – reduced my portion sizes.
5) I ATE WHATEVER THE DUCK I WANTED – and let myself be human, knowing, that by reducing my portion sizes slowly over time, my stomach would get smaller and my brain would form neural pathways would make NEW thought processes that would become my habit.
6) I didn’t have to do anything else. I don’t have to do anything else. Ever. Neuoroplasticity has ensured that I never
have to try to diet again.
In more detail and for the science, keep reading. If you’d like to read the whole science kinda thing, and check out the papers behind this – check out my 40 page book which summarises all of this (all free, lol, I should monetize this to grow it, but I’ve got no time and really would only monetize it to reach more people).
But yeah. I hope this helps. Email me if it does or if you wanna talk anytime.
# 1 – I Told Myself that it Would Take Time
–> This is one of the most important realisations you’ve gotta make. No matter how much we want it to, results don’t come in a few days. But they do come.
The trick is to not only remind yourself of this – but to keep looking at the big picture, on your entire journey – as this will make maintaining changes easier to accomplish. Instead of falling down in a heap if you can’t resist that desert at a party, you’ll remind yourself that the amount of times you had been good, and that in the long run, you were on the right path.
The science only helped me further believe, hell, it made me KNOW I could do it. But I mean it only made sense… I was only beginning my journey to get healthy – I was starting from scratch. It would take time to get to where I wanted to go. It wouldn’t happen overnight.
But that wasn’t a bad thing. I mean, it’s simple statistics. If I did things generally right, over a long period of time, I’d get to where I wanted to be. And by looking at it this way, I wasn’t forcing myself into doing something I didn’t want to – I was ALLOWING MYSELF TO BE HUMAN. knew I wouldn’t give up, or worry, or hate myself if I had a few slip-ups on the way either.
That’s exactly how you should look at weight loss, or any goal for that matter. It’ll give you the best chance of getting there (and of staying happy on the way too).
#2 – I Took A Step Back, and Made SMALL Changes To How I LOOKED At Food
–> Instead of making huge, drastic changes to my diet, or instead of starving myself, I
- Took a step back, and
- Questioned my current habits, until I saw
- An alternative perspective, or way of looking at things, that would leave me healthiest
A self-distanced perspective is described as that of someone looking at themselves as if they’re a fly on the wall. In the short term, this stops you from reacting emotionally, it reduces blood flow to limbic centres – it makes you more logical – and in the long term, it stops you from ruminating, or lingering over, things you can’t control.
When you do take that step back, your medial pre-frontal cortex, which, when firing, is associated with feelings of negativity, fires less. It’s shown to increase the ability for depressed people to think more broadly, and fixate less. It’s shown to make you more objective – you’re more likely to understand, and be realistic about things like understanding your chances of winning the lottery by doing it. Older adults, demonstrate lower blood flow to emotional centres of the brain and because of this, are what we call wiser – more logical, less likely to react emotionally, and they’re also more likely to be happier too.
You’ll get the person most likely to motivate you on your side –
YOU.
Motivation works best when it’ comes FROM YOU!
3) I learned about how neuroplasticity worked, and made it MY HABIT to look at food in the most healthy way.
This is the most important step.
Key to this whole process’s success, is reinforcing this. Walking through that thought process over and over.
Neuroplasticity, can basically be broken down to this principle. “Neurons that fire together, wire together.”
Your brain sends signals in coordinated patterns. A thought is merely the combined, coordinated firing of a chain of connected neurons. The connection points are called synapses, junctions, into which pour ‘neurotransmitters’. Neurotransmitters attach to receptors and basically enable electrical signals to pass between two neurons.
The more these synapses fire, or the more these junctions have neurotransmitters ooze into them, a process called “long term potentiation” occurs. Neurons become more and more likely to fire together, because an increased exposure to neurotransmitters leads to less neurotransmitter being required to mount the same response next time (‘refiring’ lowers the threshold to allow a connection to fire), and also creates a larger impact when a signal is given.
Over time, a group of neurons firing together which underlie a movement, a habit, or a thought process, solidify into a cortical map. This video outlines this in easy to understand principles. If you’re keen – go watch it (remember, the reason why I outline all these things is so that YOU understand, and thence, can SEE how this process will work in you, making YOU more likely to succeed).
When you practice something, be it learning to shoot a basketball, a ditty on the piano, or to create a new habit, it’s hard to even coordinate an action at the beginning. But the more and more you do it, the easier it becomes. At a cellular level, this is because those synapses that create the desired effect – of you getting a shot in, playing the right notes, or remembering to put your keys in that one spot – as you’re trying to do them, become stronger than that of you missing, stuffing up or forgetting.
That’s how your learn.
That’s what neuroplasticity is.
Thinking takes effort. It was suggested that chess grandmasters burn up to 6000 calories per day while playing. Though a gross oversimplification with broad assumptions, it’s very much true.
Neuroplasticity is basically your brain making it easier for you to access a thought you use often. When thinking “Why am I eating this?” for a few weeks (and it only takes 3 – 6 weeks to develop firm neural links that are Harder to break than bad habits), it’ll become so easy it becomes automatic. You’ll find yourself asking yourself “Am I really enjoying that last bite?” and “Am I really valuing the extra $0.005 of rice I’ll throw away here, more than the hundreds of thousands I’ll spend facing coronary events in my 50s or 60s?” ALL THE TIME.
It becomes easier to fork out one less spoon, pick the healthier option, or just enjoy a few chips rather than scoffing down a packet, than it is to do the opposite. Doing the opposite won’t even make sense.
They key to making it through the 2 weeks?
Rewarding yourself, over and over, and allowing yourself to be human too!
Neuroplasticity is the foundation of learning, memory and habit formation.
And it works best when you give yourself a GOAL to accomplish, and get there by reaffirming BEHAVIOURS which eventually solidify into THOUGHT PROCESSES that become your habit.
That’s where reinforcement of the above ‘process’ of
1) Taking a step back and then
2) Breaking down your major obstacles into chunks that you can counter and follow
Is one that you need to practice.
Let’s use muscle memory as an example. Sure, it’s easy enough to visualise a goal of increasing your first serve percentage in tennis. But you have to serve over and over to create connections between your cerebellum and cerebrum (major parts of your brain that are responsible for coordinating movements), and solidify them as an automatic process.
Self rewarding is key to focusing the effects of neuroplasticity. When you pat yourself on the back, you release dopamine which solidifies neocortical maps as they form.
And as stated earlier, not only does self affirming, rewarding yourself when you get closer to your goal with a little “YES,” lead to dopamine firing which focuses neuroplastic map formation, the closer you get to a goal, the more dopamine you fire as you get there. Meaning it actually becomes easier and EASIER to maintain a habit the longer you do it.
It’s why, when you have focused and gotten a few good serves in, the next few become easier. The more and more you practice your serve, the higher and higher your serve percentage goes up.
When you combine this with you not being too hard on yourself… it creates an amazing feedback loop of you continuing to pump yourself up, pick yourself up when you need to, and you relishing as you grow and grow and grow.
So don’t feel too bad if you do eat a little bit more one meal. Because in the LONG run, as long as you make positive decisions, you have no way to go but become healthier and happier.
Neuroplasticity, self-rewarding, and goal setting is key to weight loss.
But what actual “hacks” can you use to get your mind on your side? That’s what the next section is about.
4) How to actually Hack your Stomach, and Your Brain on Food?
i) Reduce your Portion sizes. SLOWLY:
When trying to reduce how much I ate – I realised that, especially with foods I liked, I was just gulping down food down by the spoonful. But in truth… I wasn’t really taking the time to savour them. The first 5, 10, maybe 15 spoonfuls or bites were most enjoyable. The last few… even with my favourite foods, well, to be honest, I was really only trying to finish off what was left.
To change that I made small gradual reductions to my portion sizes. I started savouring my meals and once I realised I was full, I’d just leave it, put it in the fridge or throw it out, and next time take out less.
Over time… the portions got smaller and smaller. When going out… if I didn’t really feel like finishing off my plate, I’d just leave it and ask if anyone else wanted a few bites. I was brought up on the whole “Finish your plate, there are children in Africa who’d KILL to have what you’ve gotten!” sort of mentality… and it’s true. We waste tremendous amounts of food, and do need to respect it more.
But why was I destroying my veins, my health, my vitality to assuage this preconception, when I could instead just take out a few less spoons, order a medium (and in time, a small) meal instead of a large one, and pack away good meals for breakfast or lunch the next day, and feel better for it?

Your stomach usually has a capacity of 200mL, but can stretch to hold up to 1L in most humans, by relaxing smooth muscle cells which comprise most of its wall. Over time, however, if not stretched to larger limits, the stomach loses the number of smooth muscle cells, and pacemaker cells (those which cause coordinated digestive contractions), leading to lowered capacity to relax. Furthermore, levels of neurons which release nitrous oxide, which promotes relaxation of smooth muscles, also reduces in patients who have lost weight recently.
So over a period of a few weeks, slow, sustainable reduction in meal sizes will cause you to lose the ability to eat larger meals over time!
It’s interesting to note that even after a while of this kind of fasting, even after overconsuming, average stomach stretchability did not return back to normal levels, meaning you’ll have the ability to have the occasional splurge without starting back at square 1 again.
But key to all of this working is the neuroplasticity of your mind. It’s widely conceived that you need huge willpower to resist the temptation to continue eating. But the simple changes in the way you think about food described above is what ensures you’ll get to that stage where your stomach adapts.
Neuroplasticity is the brain’s ability to form new cortical maps – linkages between series of neurons – in response to various scenarios. ‘Neurons that fire together, wire together,” is the basic principle on which this idea is built – so reminding yourself that
- You like food, but hate that fatty, full feeling afterwards
- You like food, but often shovel in the last few bites just for the sake of it. And that
- You enjoy meals even more when you really take your time to savour the meal
for just a few days in a row, will start forming these cortical maps. In weeks, these cortical maps become so solidified and prolific – they become your automatic response. You won’t have to think these things anymore, you’ll already, subconsciously believe them. And though weeks of resisting temptation seems hard to do, because it
- Is coming from YOU telling yourself these things;
- Because your cortical maps are forming and becoming more and more solid over time, and
- Because you’ve got a long term goal, which causes more dopamine to be released each step you take towards it –
it’s actually quite easy to do. They’re subtle, small changes to how you view food, but combined, they make a HUGE difference. It’s the difference between going into a diet, hating life and having to force exert significant willpower to control yourself, and eating what you want, but slowly, and surely, changing your mindset, and letting your brain lose the weight for you.
Remember, thinking is HARD. We’re lazy, and we don’t wanna work, because your brain consumes oxygen. But if you understand HOW the brain works and learns (pretty much everything we do and get better at relies on this neuroplasticity), and you make changes that make your NORMAL thought process a HEALTHY one that DOESN’T REQUIRE willpower to do… Well being healthy BECOMES the lazy, easy thing to do.
And you know what? It worked. In January this year, I could eat a whole pizza, and I’d go up for second servings when lamb curry was made at home. Now… I can still do a half pizza… maybe more, but only when I feel like it. And I barely finish 3/4 of a plateful of rice and curry (I used to eat 1 – 1.5 lol). That small change in mindset resulted in a huge reduction in my calorie intake per day. And it’s the main reason why I’ve lost so much weight AND KEPT IT OFF without trying.
ii) Making Healthier Choices:
Me – I’m a foodie. I like trying different things, new cuisines. And I like variety in my day to day life. I also like my meat, hate salads on their own (chemo’s changed my taste a lot – I used to love the taste of lettuce… now it tastes like dirt at times) and I like eating carbs like bread or rice with meals. Who doesn’t really?
With these simple changes, I was able to eat all these things and still lose weight.
But I knew I could stand to benefit from eating generally healthy foods… so again, I took a step back, questioned my current habits, and made small changes to my mindset on food, which helped me eat more healthily too, without depriving myself of the pleasures of life.
Carbs… I did like them, but what I liked more was what I was eating with them.
So I changed the portions around, added more fillings or curries, whatever I was eating at the time and reduced the proportion of that to however many slices of bread or spoonfuls of rice I’d eat with them. Again, this happened over weeks, not instantly.
With salads, whose taste I couldn’t stand post chemo, I started drizzling, sometimes dumping tasty dressings based in oils (luckily regular olive oil is good for you), and added things like cottage cheese or olives to make them tastier.
Juicing, though it gets good vitamins and veggies/fruits into you, was too much of a hassle to do regularly, especially cleaning the damn things. So I started looking around for good fruit/vegetable juice mixes with no added sugar or preservatives and came across this brand, which uses pressure instead of preservatives, and doesn’t add sugar to the mix and saves me time too. There’s bound to be something similar in your location!
I liked variety in my diet, and that was good. So I picked cuisines to eat regularly that were easy to prepare, and tasted good and were still healthy for me – things like tacos or stir fries (which have good amounts of veggies, are easy to cook, low in carbs and have good, but not excessive amounts of meat) and I mastered them. They’re like a staple to me now. And I don’t hate eating unlike most people who diet – so I maintain this healthy lifestyle still, to this day.

I couldn’t believe this came from CostCo either when I first tried it. But I highly recommend it – their Kale/Sweet Potato/Quinoa cous cous salad.
iii) Taking out the Junk Food
To be honest, I haven’t taken out all junk food. I probably eat junkfood once a week now, still. But I lost all that weight while eating junkfood every few days.
Still. Junk food is junk… food. How did I reduce the amount of crap I ate?
Well I mean I looked at them, from that step back, and asked why I used to have that crap so often… I mean they do taste good, and they are cheap and easy to prepare… But I hated that “fat”, “oily” feeling I had after eating a packet of chips, some chocolate or a burger or box of chicken from KFC.
I didn’t cut them out entirely, which many people do, instead I only got a few small bits and pieces from fast food places or fish n chip shops, every now and then, and had them alongside other, healthier stuff. KFC – I made sure I had that with these pre-made salads I found in CostCo which complimented it perfectly. With the chocolates, and chips, instead of gulping down a handful or packs of tim-tams at a time and then feeling bad afterwards, I shared them around with other people, or scabbed a few chips or bites from friends instead of buying a full pack and feeling like I had to devour it. Those small changes made me eat healthier (and also saved me money too – sorry guys). I still got to enjoy the taste. But I sidestepped feeling crap!
They are easier to cook, I guess, and many people just don’t have enough time to cook – but those meal suggestions I made above really help with that. Another thing that makes cooking easier for me is marinating meats and eating them with salad or veggies or a good slice of cheese (which acts as a side dish for me – I love block cheese and it’s high in proteins too so it makes you fuller quicker). I marinate a huge amount of meat in tandoori paste, or honey soy dressing – whatever I feel like – leave it over a few days (the longer it marinates, the better it tastes) and cook it in meals with this simple frier/grill which only requires me to flip once and makes meat really tender too and it’s done quickly. It’s quicker than a drive out to the closest McDonalds, and takes only a few flips in total to make it.
These small changes to how I viewed eating, small changes to my mentality, was all it took to improve my diet drastically. I haven’t cut anything out, I’m not hating myself and making myself less likely to succeed by following strict diets and better meals is a MAJOR reason why I’ve lost so much weight and why I’m so healthy right now too!
Improving My Fitness/Exercise Habits:
When I started trying to get fit after my second transplant, a year ago, I told myself I was going to take it slow and build up from there. After my first transplant, I pushed straight into weights and basketball, I didn’t even focus on getting any endurance back before doing so and in the end, it didn’t help me get healthier… It just made me frustrated (because I wasn’t improving much) and probably made me sicker overall too.
This time around though, I didn’t have a relapse, and lower blood counts stopping me from improving. What I did have was excuses and laziness and self-consciousness about my abysmal fitness, which made me not train consistently, which made me frustrated that I wasn’t getting fitter, which made me lose the will to get fit – initiating a huge cycle where I’d get motivated and exercise for a week or two and then stop, only to repeat it, again and again.
iv) Taking that First Step.
Well, changing how I looked at things helped me get more consistent in my training. Motivating yourself to get off your bum and start is the hardest thing to do when exercising. But by changing your perspective on exercise, from a thing that is painful and excruciating to do, to something that you can build up on – something that gives you more energy throughout the day – gets you over that initial burden of getting up and doing that first set. Looking at your long term goals becomes really important here. Remembering to focus on the fact that you will get there – in time – as long as you’re doing the right things OVERALL, as opposed to expecting to beat your PB every session, ensures you won’t give up when you face failure – instead, as you’re prepared for these, you’ll be picking yourself up.
It’s when you have a bad, or disappointing workout that this patient thinking really helps. Instead of getting down and sad about it – you’ll be ready to go the next day, because you’ll know for that 1 bad workout, you’ll have 5 other good ones, and you’re still be heading in the right direction.

Another great tip – do something FUN! You’re much more likely to commit, and form good habits, if you make yourself accountable. So get a gym buddy, or join a team! 3/4 adults played sport growing up, but only 1/5 play as adults. Why is that?
Start Easy and Build Up From There
When building up from scratch, which I’ve had to do plenty of times, looking in the long term REALLY helps.
In my case, and that of many other patients who read my blogs, treatments and concurrent infections would bring me back to starting position, walking and body weight exercises were excellent in building me up. I started with push-ups, squats and sit-ups in front of the TV. Those things gave a good burn and made me feel like I did something and gave good, constant improvements when I did them consistently too. I didn’t just like walking for no reason, so I used my mind and my interests to my advantage and started walking down to the river with a rod in hand, looking at the tides, watching the small fish and how they moved, and getting good ideas and experience to improve my fishing. Basketball – my favourite sport – always keeps me motivated, and watching a good basketball video or movie would always get me up and ready to have a shoot around. You can use whatever passions you like. Cycling, rock climbing, diving, whatever you want to motivate you to keep you in the gym or in the pool or on the track.
Make exercise time valuable. I know many students find it hard to sit down and study – so download your lectures and put them onto your music player and go for a walk or run. Same thing goes for podcasts of your favourite radio shows, or just blasting your own music. Makes it easier and even fun to train – in fact, Jana Pittman, a classmate of mine does this to keep up with medicine and still train at an Olympic level.

The power of incidental exercise doesn’t just stop at boosting the calories you burn a day, but also extends to formulating strong, neuroplasticity-moulded, attitudes towards exercise. Each time you pick the stairs – you make yourself more likely to pick them next time!
Don’t Be Shy, Or Worry About What Others Think of You
Taking that first step was hard for me. After chemotherapies, where I’d have to start from scratch, I’d always feel embarrassed and self-conscious at how little I could do, and also about how weird I’d look. You may feel the same way when someone racks up more weight than you can squat on the bench press, or when someone laps you in the pool or when someone blocks you on the basketball or volleyball court. Whenever I wanted to work out, I would always feel the stares of others on me and that stopped me from wanting to go out and get healthy in the first place. When you take a step back and see it in another way though, you’ll see that you’re stopping yourself from being the healthiest and happiest version of yourself because of what other people may be THINKING about you. Read more about how I managed to get past my self consciousness and become the most confident, happiest version of myself here.
Overall – losing weight and getting fit and healthy is NOT something hard. The only thing standing in the way of you getting there is YOU and your mindset. Get your mind on your side and the rest will become easy.
Those fad diets and boot camps can help lose weight and they do work. But they’re not easy to maintain – they’re not for everyone. Using your mind to your advantage is the best thing you can do to help you get healthy.
I wrote this part in April 2016. I went from 97kg in November 2015 (after I gained bout from that third bout of cancer) to about 80kg now. And I’m in that luxurious position of needing to gain weight.
As of Sept 2021, I’m at 74kg. I haven’t ever tried to lose weight.
Feel free to leave any tips of your own down here. To help me and others along on their journey to get fit and healthy.
And sign up to my email list (I don’t post often, but you’ll be notified when I do this way!).
Bone Marrow Transplants
The bone marrow transplant procedure, in a nutshell, is basically getting someone else’s blood stem cells (haematopoiec stem cells is the technical name), located in their marrow, and infusing it into you, so it settles. They aim to get someone else’s immune cells in you, to kill off your cancer (your immune cells are made by your blood stem cells). And the major side effect, other than the dangerous infections you can get during the procedure and in the first 30 days due to, largely, chemo, is graft versus host disease, which can last a long time in others (but in small doses, is actually a good sign the process is working).
How it works for the donor – it’s taken peripherally from the arm, after getting a medicine which makes those stem cells enter your circulating blood for a few weeks (click here to learn about that).
On the recipient’s end, you receive it through an infusion into your veins, in most all cases. It eventually finds it way into your marrow and starts producing your donor’s blood cells (including white, immune cells), after a few weeks (it took 3 weeks for mine to engraft on both occasions, but it can vary).
The idea is, though you and your donor are matched as well as you can be – there will always be slight differences between you and them, which makes them recognise cancerous cells and kill them off, where your immune system may have lost the ability to do. This is a good thing in that it’s how the BMT or SCT (stem cell transplant) is supposed to work. But it also is the cause of the major side effect, graft versus host disease, where your donor’s cells attack your own organs. I’ll get to that later, here’s how it all goes though.
Prior to the transplant, you receive workup of some kind – often they want to ensure your underlying disease is under control. If it’s a blood cancer, often that will involve chemotherapy. Once they have the disease and any underlying conditions mostly under control, and they find a match, and coordinate timings (usually, you want to get the donor’s cells into you as soon as it’s taken from them), they begin the workup to the actual stem cell transplant process.
Usually, a week or so before, they’ll begin immunosuppressive regimens and chemotherapy that are designed to kill off your current immune cells. In younger patients, they may also offer total body irradiation, which is a high dose of radiation given to your entire body (in younger people, marrow can be produced all over the body, so all areas are targeted, though they will provide shielding to your brain and lungs, in most cases). The idea is to kill off your old bone marrow’s cells and replace them with your donors’.

I won’t lie, the BMT process and chemotherapy is tough. But it is lifesaving. Definitely listen to your doctors!
During the next few weeks, like many chemos, you will have a lot of your immune cells and your blood cells obliterated. So you’ll be very susceptible to infections. It is very important to do everything you can to avoid infections in this time, from limiting visitors (especially sick ones), to cleaning and bathing regularly (even when you won’t feel like it) and following your doctors’/nurses’ orders. You also may experience other side effects such as nausea, gut pain (from your stomach lining cells dying off), fatigue and general unwellness. There are many chemotherapy specific side effects too that may occur, and you may also get other side effects – eg. with TBI (total body irradiation), you often get mucositis – inflammation of your mouth and throat – which can be extremely painful. I’ve personally experienced this myself and highly recommend you follow doctors’ suggestions and get ENG tubes if they think it’s appropriate and helpful, and getting pain teams to come in and help too. Having said that – my second transplant was a ‘reduced intensity chemotherapy’ regimen. I only had nausea and didn’t get an infection once, and it went quite smoothly compared to the first. Everyone’s different, every regime is different, and even in one person, at different time points, you can react differently.
Other things they may do in your workup/the month before your transplant, is check your heart, and lungs, and, if you’re in that age category, your fertility. They’ll put a line in just before they begin treatment in hospital, this may be in your arms, or via ports they put into your neck. During the transplant, and the immediate transplant workup, they’ll watch over you, do bloods regularly, get scans when required, and treat things like infections. Infections are often the most dangerous thing you may face, but they’ll be sure to give you antibiotics, and other treatments, as required during this time frame.

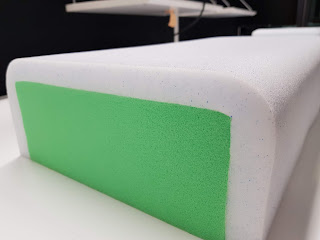
This is the TBI – total body irradiation process. This is usually done in younger patients, as they are more likely to have marrow that persists in other bones of your body (adults often only have it in their sternum and hip bones). Hence why they shoot radiation at your entire body (left of this photo is a machine which does this). The rice bags keep you still and provide some protection to important organs like your brain and lungs. And they keep you still. It lasted 30 minutes, and I had 5 sessions over a week at a special clinic the week before my transplant). Straight after you may get a burning sensation in the skin (this is resolved by creame in most cases). The other common side effect is mucositis, a sore throat, which can be very painful. So listen to your doctors if they recommend a feeding tube! I learned that the hard way!
At some point, often 3 – 4 weeks after “Day 0,” where they infuse you with your donor’s cells, you’ll ‘engraft’ and have your donors’ cells start making cells in your blood. They’ll be monitoring for this. After this, a good number of people get acute graft versus host disease, which can affect any of your organs, and can be pretty severe. This occurs in the first 90 days usually, and can affect any of your organs – from your skin, to eyes, to liver, to gut. I personally had bad skin and liver and gut GVHD (in my first transplant, I had skin and liver aGVHD, and in the second, liver and gut aGVHD). Not everyone gets GVHD. It can be a good sign that you’re getting the ‘graft versus disease’ effect too (where your donor’s cells kill off/stop your cancer cells from returning), but too much GVHD can be bad too. Your doctors will treat you after you engraft with some medicines that suppress your immune system – often cyclosporine, but different doctors/patients use different treatments. If GVHD manifests and gets severe, they may add more or increase your dose. Or they may reduce them over time.
You’re still not out of the woods after this time frame. You can get infections, still. And with GVHD – days can be critical when it comes to your outcomes, so make sure you tell them of anything you may experience. With different organs, you may experience different signs. Eg – with the skin, you may get rashes or feel like your skin is burning. With the gut, you may get diarrhoea, sometimes constipation. With the eyes, you may get burning or find it difficult to open your eyes (which may be due to skin GVHD affecting the skin around your eyes). It varies from person to person. It’s VERY important you see your doctors if something happens. But sometimes, you won’t feel anything. With my liver graft versus host, I didn’t feel a thing, but had very very high liver enzyme tests.
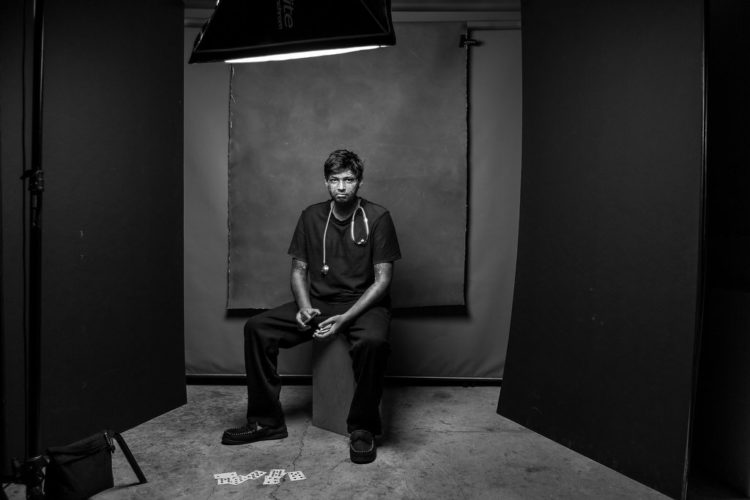
I couldn’t find a clean, clear photo of my skin, so sorry for the captions. But this is chronic skin GVHD – I have quite severe chronic GVHD and it’s not too bad, other than the looks (I don’t mind the looks though – this is how I dealt with the social anxiety that comes to many post transplant, due to the change in looks). Acute skin GVHD can be more red and flared, and may occur anywhere. It may burn or itch. I know it’s hard, but try not to itch! But right now, as someone with chronic graft versus host disease, I can’t feel it, it isn’t painful, but it may make my skin less elastic, and does impede my joints a little bit. But I’m largely OK now!

Usually, they’ll tell you to come into hospital as soon as possible if you get a fever or infection symptoms of any kind. With COVID-19 going on right now, clarify with your doctors if or when to come in. Many hospitals, including mine, will give you a card to get you into ED faster. Even after the pandemic ends (which may not be for years officially), it may be wise to wear a mask and avoid crowded areas too.
Depending on your donor and your status, you may also get exposed to viruses that may put your graft (your transplanted cells) at risk. Your doctor will likely have you on prophylactic, preventative, antivirals, antibacterials, and maybe antivirals too to prevent this. And they’ll likely check your levels of various medicines, and monitor for these viruses too. This is why it’s really important to see your doctors and get your blood tests as much as they want you to. Hopefully, this will go from weekly appointments to fortnightly, to monthly, to 3 monthly, to yearly. And then comes long term monitoring.
You also generally feel tired. I did after both transplants for months. Some of the medications you may be put on have annoying or frustrating side effects – eg. prednisone is a steroid medication (not the muscle building type unfortunately), which can make you angry, make it hard to sleep, and make you gain weight. But it’s also lifesaving. It’s important to keep in touch with your doctors to monitor this.

The way cancer changed me used to really impact my mental health. To the point where, even though it was harmful for my health, I didn’t want to go out because of how it affected my looks. This is me years afterwards, but straight after chemo, on 100mg of prednisone, I had the classic “chipmunk face.” But I got over that after a while. This is how. I hope it helps those of you who may suffer from this out too.
After 3 months, you may also develop chronic graft versus host disease (cGVHD), which may manifest all over your body, and may get severe too. it’s important, once you get signs of anything weird, to tell your doctors about this so they can treat it, again. And treatment may last longer or be chronic, as the name implies. I still have some, 8 years out. But again, everyone’s different in this. I’ll make a post about this later – but there are many organs it can impact, from your skin, to eyes, to lungs and in rare cases, even heart. It’s important to get on top of this early. But the good news is, in many patients, it either ‘fizzles out’ or ‘plateuas.’ But without treatment, it can worsen, even after you’ve got it under control. So stay connected to your doctors and listen to their advice!
That’s the transplant process, in summary. I know it’s a lot of information. But the main thing, is it a marathon. But it is also curative – it was one of the first curative options we had for any cancer. Though it can be dangerous, it has a good chance of fixing many diseases. Your doctors wouldn’t be doing this to you if they didn’t think it could help.
I hope it makes sense. Let me know if you have any more questions. And sign up, do email me at info at nikhilautar dot (com) with any questions, and stay in touch!
And then there was last week.
I’ve been to ICU at least 4 times. I remember 2 of them. I may have been there more during chemotherapies. But this one was the one I remembered most.
The last time I was in ICU, how I’d felt.
Hospital is a scary place, in general. When I realised I had unstable angina, and then, shockingly, found out that I was a walking talking heart attack risk… I was scared.
But the way I deal with all this stuff is to try and take a step back, and logically reframe the situation I’m in. I challenge the fears, doubts and worries I feel. Keep challenging them from different angles until I find secoond pathway, or way of thinking, that would lead to the highest chance of me being happy, healthy, and sane during a treatment.
I was good at this when I started chemo. It became my norm. But there was a time when I’d gotten bad at this. I’d had a few bad experiences in the past with doctors. I used to catastrophise when I came into ED, always thinking the worst – worried about infection, my one, remaining eye blowing out, what could be happening. Anything could, right?
But I’ve gotten better at dealing with that. Psychiatrists have helped me heaps in doing that.
But there was something about this hospital that made it that much easier.
From seeing my friend, in ED, calling out, and him assessing me as Cat 2 (I honestly just wanted to say hey!), despite the receptionist receiving a letter indicating how urgent my situation was.
To when I got my angiogram. I knew at that point something was up. But to see that severe an occlusion was a shock.
But the reaction of the cardiothoracic team, and Dr H in assuring me of what I knew, that I couldn’t leave at this point, until we’d done something, assured me, yet again. I know the hospital’s reputation and that of the ICU, but the calm, cool collected measure of how Dr M presented himself, made me even more assured.
Then my cousin started pointing out that this could possibly be more complicated than your regular CABG. But your prompt responses in replying to his concerns and getting a second opinion from St Vincent’s Transplanters left me, yet again assured that I was in good hands. Prior to surgery, I was largely thinking, “Let’s get it over with!” due to your team’s completely reassuring manner.
But it was the little things that REALLY made a difference. From the care and compassion shown by the nurses of 6D to give my mum a mattress – A MATTRESS – when in every other hospital, we’d been gently nudged towards the door, given sofa beds where they had them, or in some hospitals’ cases, them forcing Mum and Dad sleep on 2 chairs opposite eachother, even in the direst straights… we got a mattress.
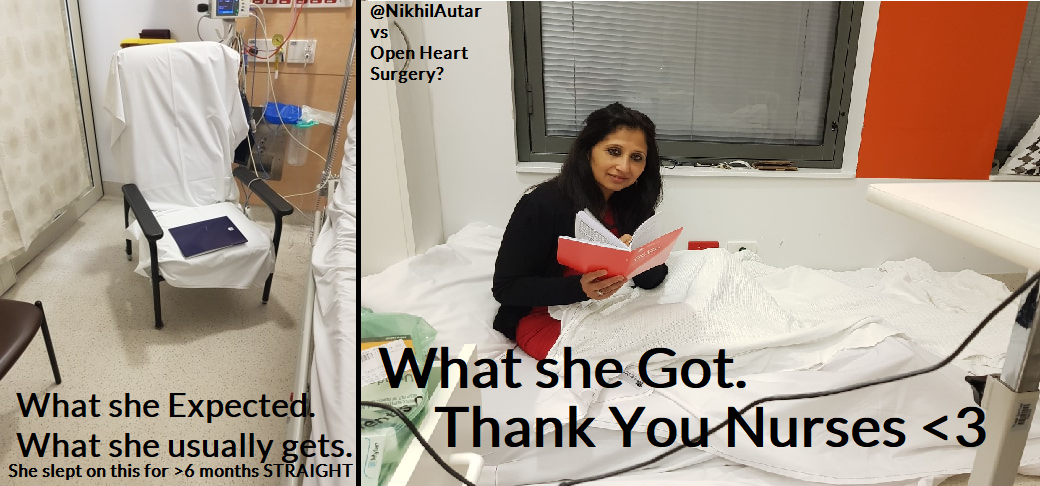
The dignity that little actions like this, and the providence of carer meals – carer meals – who would have thought… made me assured too. Not just because my family was being cared for too, but BECAUSE they were being looked after just as much as me. It really signals to me that you’re doing something good… and upholding a set of amazing values that is embodied to the core, at this hospital.
THAT is just as powerful as confidence in your medical abilities to someone who’s suffering, and scared. Please, never underestimate the power of making people feel CARED for in your practice. It was only the knowledge that there was a doctor across the road who cared for me that stopped me from walking, instead, in front of a train a few years ago. A decision that’s led me to get professional help and get my mind back on my side, as it had been before chronic pain and depression.
It’s something I’m assured, by the way you took care of me, that is not gonna be an issue for wards 6D, E and B (and wherever else I may have been). You guys already have this on lock.
To the doctors, thanks for your calmness and reason and thoroughness.
To the orderlies, dietitians, physios and everyone else, from cleaners to admin staff, thanks for not only being extremely professional at what you do, but also human and funny too.
And to you guys, my favourite of all… the nurses…
Over the years, through crisis after crisis, and challenge after challenge… Through near death experiences, and near death-from-boredom ones during hospital. You’ve not only been a barrier between life and death for me, but also a barrier between sanity and insanity. People call me an inspiration for how I process things, how I try and be pragmatic, to do whatever I can and then sigh and say “I’ve done all I can, what’s the point of worrying when there’s still a chance it could work anyways?”
But I can only be this way because I’ve had these amazingly compassionate, caring people on my side during every crisis in my life.
When I’d heard that it was the ICU nurses who addressed tamponade as well, I was shocked at first, but not really surprised. I know nurses who’ve set up clinical trial facilities for whole health districts single handedly. A nurse friend of mine lectures doctors and nurses internationally on CVC placement. This is just more proof of what I already know. That you guys ROCK.
Your technical skills and knowledge are often just as much as doctors’ own, but your ability to care, to go the extra mile, to be compassionate, show humanity, and humility amidst everything is your TRUE power.
And you’ve demonstrated to me, yet again, that YOU are the backbone of this very healthy system.
As a future doctor, who’s dreamt of becoming one since watching Hawkeye Pierce perform open hand massage in an episode of M.A.S.H, I’m yet against convinced that you nurses are just as much, if not more, the REAL doctors of this unit. You nurses in particular inspire me to want to do better, and be better. To keep trying to help people as much as I can.
You guys at Royal North Shore, are somehow on ANOTHER level.
I can’t thank you guys enough for what you’ve done for me. If there’s any way I can help, let me know.
Do have a read of NikhilAutar.com/nurses on a bad day, or of my book, NikhilAutar.com/mybooks which you thankfully did not make into the memoirs of an ex cancer patient, medicine studying, medical researchering, poker playing, startup creating kid, but rather one with many more chapters yet to come.
Forever in your debt…
Nikhil Autar, and family.

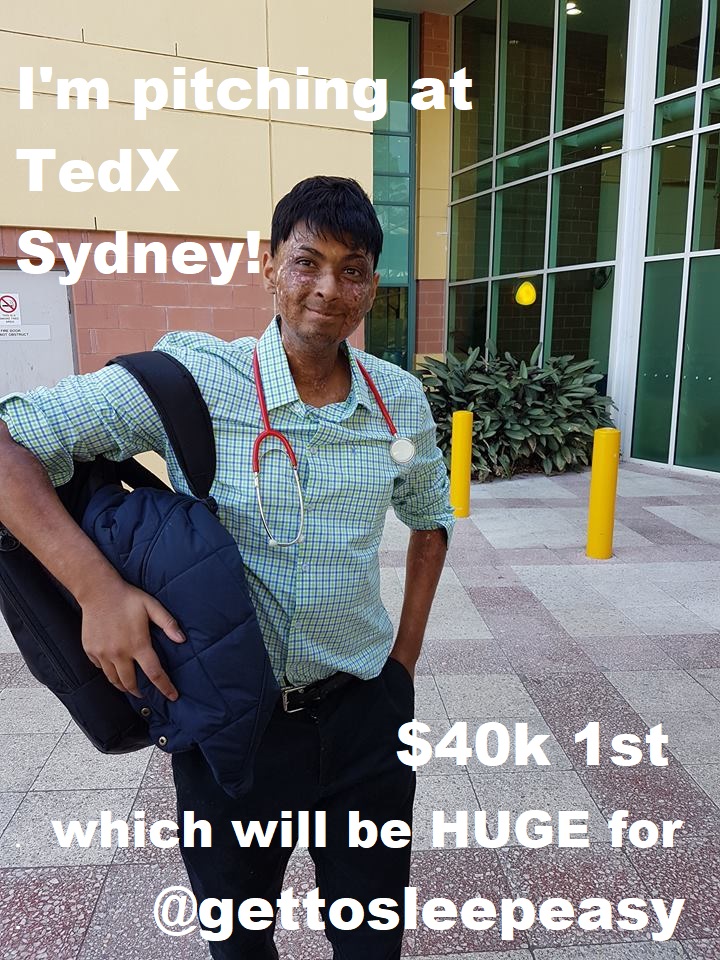
It’s a competition called St George Kickstart, and TedXSydney is one of the biggest franchises of Ted out there. It’s such an amazing honour!
When I started out trying to find a solution to this invidious problem of #preventablecomplications (falls, pressure sores and pneumonia), I knew it was a big problem.
When we started talking to nursing homes and hundreds of caretakers, doctors and nurses homes, we knew our Smart Inclining Bed would save lives.
And now we have an opportunity to present in front of thousands of changemakers and to win this prestigious prize that will allow us to clinically trial our products and get it to market faster.
I’m stoked. Looking so forward to it. And excited about the further impacts we will make!
GetToSleepEasy.org to find out more about our #SmartIncliningBed and how much of an impact it could make… not just to vulnerable people’s lives, but also your sleep (and your neck when you Netflix in bed ![]() ).
).
If you wanna have a look at my script and give me feedback in preparation for this – please check it out by clicking this link. You can leave comments and advice there, for sure! I’m looking forward to receiving any and all advice regarding this!
Also – sign up to my email list to keep updated on this, and on other things medical, funny and me!
[email-subscribers namefield=”YES” desc=”” group=”Public”]
Check out what we do at Get to Sleep Easy in this sweet little demo vid below!
]]>
So, what are we doing?
So where are we? What comes next?
Well, in a completely separate competition… we may be getting flown out to become GLOBAL Student Startup of the Year (that’ll be amazing). We’ve got working prototypes which we hope to test with our amazing nursing home partners in 3 – 4 months time. For reference, we’ve got a device that converts any bed into a hospital bed for 1/10th of the price and smart sensors that detect and prevent falls, pressure sores – even if someone’s stopped breathing (let me know if you’d like to test these, or get one for loved ones!)! We’ve got opportunities to jump into some prestigious business accelerators which will turbocharge our progress, for sure.
Other updates!
My research – I’ve completed the degree/exam components! Now I’ve just gotta deliver my research project to graduate from that research degree! Hopefully, sometime over the next few years, I’ll be healthy enough to get back into the wards, but Get To Sleep Easy, if we keep going the way we’re going, will ensure I can keep making an impact, no matter what!
life.
I’m sure many medical students and doctors would tell you the exact same
thing…
For me it was personal.
I’d always wanted to study medicine. What better job was there? You could save lives
and live in relative comfort your entire life. I’d get to emulate my childhood
hero growing up, Captain Hawkeye Pierce from M.A.S.H.
But after leukaemia struck my life… it became personal.
I wanted to help people as I’d been helped. It was my doctor’s words; that
“The Good News Is You’re 17 and You Have Leukaemia, but the Bad News is
You’re 17, And You Have Leukaemia…” and his actions that got me to
believe that I actually had a chance in this… It was another patients’ words
the day before my transplant that really sunk in, and changed my life. Imagine
being in a position to do that for people everyday!
My first day in medicine was one of the most joyful of my life.
I was so excited to finally be in a position to give back, and so delighted to
be alongside so many other people who cared just as me.
But as time went on… things changed.
For me, and for many of my classmates too.
As I progressed through the course, I got more and more burdened with work, and
more and more dissatisfied, and indoctrinated (pardon the pun) into the collective Group-Think of
modern medicine. One which emphasised speed over accuracy, marks over
competence. One which measured success through KPIs such as reduced wait times
and greater efficiency rather than reduced morbility and morbidity, and higher
patient satisfaction and involvement. As I feel many in this profession feel at some point.
mental illness, and the fact that they are illnesses, not just an abstract
constructs or “excuses,” as many still widely suggest and believe.
Somehow still, amongst those with depression or severe symptoms of
depression, only 15% of medical students actually get help… For doctors… the rates are even lower.
Why is this happening though?
Aren’t these people being paid heaps?
Don’t they know the risks of the disease, and how altered biochemistry can
alter your very mental state – your very person?
Well, there are many reasons why.
Various personality traits and attitudes make doctors more likely to suffer
from depression.
Perfectionism, hints of narcissism in some, compulsiveness in others, martyrism in most, and disparaging views of
vulnerability are all commonplace. Facing death, watching good people suffer, and losing
the battle over and over again also burdens doctors. Burnout from stress affects 45%
of doctors, ladies and senior physicians in particular. And as this article puts so poignantly, Osler, the founder of the
first American residency program, advocating for equanimity in physicians, was
perhaps the largest contributor to all this…
weakness is a failure on their part. A failure.
how can they serve their patients?
to bear…
lives in America alone.
worth…
Junior doctors and medical students have similarly sky-high rates of depression
and suicide ideation (the 10% figure is a conservative estimate; studies in my
nation show , but have the added pressure of exams and the weight of
expectations on their shoulders too.
first time, often overseas for many students (where the added pressure of
maintaining a steady income is another burden), high levels of student debt,
and the sheer pressure of the course and succeeding itself plagues many
students.
complain about many of the above stresses. Many feel medicine takes over their
lives. In a time where they should be out and enjoying their life, many
students, as well as doctors, regret not enjoying life more. And many feel disillusioned too. They feel they were misled
about what medicine actually was. About the impact they have. About the
difference they make. So many of my friends express this in particular. But the toxic, competitive hospital environment, where specialty spots are
limited, the medical heirachy is emphasised (and perpetuated by older doctors in an “If I went
through it, they should too” manner) and bullying is rife, also pushes many
young meddies over the edge.
Very recently, in my country, Australia, 3 junior doctors took their lives within one week.
to.
life last year.
mine.
that remains.
mental illness is one step in the right direction.
believe, discusses the expectation of doctor perfection, and how this
counter-intuitively actually worsens patient outcomes.
mistakes are their fault, a great burden is placed on their head.
this unreal expectation of perfection is what, as Brian Goldman points out
here, is only harming doctors more.
reporting of issues or near misses in hospitals. More recently, at a quality
and safety lecture I attended, I learned there was one in our hospitals in my
state in Australia, but that it was under-utilized, and something feared by
doctors, as opposed to the learning tool it was intended to be.
mistakes, and seek sympathy from other doctors, could change the lives of
hundreds of thousands of silently suffering, perfection seeking, burned out
medicos. And it could improve patient outcomes too.
Perhaps confidentially, with identification being made impossible. Though it’s
horrible that some die due to lapses in doctors’ concentration, as pointed out
in this article, overworked doctors, facing physical and emotional
stress, are less competent ones. Hundreds of thousands will die due to medical error this year alone –
medical error is estimated to be the third highest killer in the American medical
system.
mistakes, not making diagnostic/prescribing/treatment processes better, and not
giving doctors a place to vent, and relax, is only going to increase this
number if anything.
interesting man – Atul Gawande (highly recommend his books on medicine and how
to fix it), discussing a simple process which reduced mortality in surgeries by
as much as 40% – a checklist. These little innovations and improvements are
necessary to accomplish the end goal of saving more lives and reducing
suffering!
alone isn’t the only way we can ease doctors’ strife.
have to face too.
work everyday, knowing that you’re going to witness suffering, pain and death
can be soul-wrenching. I certainly do feel disillusioned when walking through
wards and seeing the same story, of a seemingly nice person, suddenly finding
their health deteriorating, and then, in most cases, having some scars from all
this tail them for life.
first. Especially when it’s someone you’ve really connected with.
can deal with it. This is how I dealt, and deal with mine though…
devastated. It shouldn’t have happened. Not just because he was so young, not just
because he’d left a baby behind, but because it was so sudden. So unexpected.
Just so unfair.
Inconsolable. But silently suffering. For weeks.
time, but I was going through depression. That was the first time I did. That
someone so young, innocent, someone who I’d helped grow to overcome so many
battles and someone who I thought would make it could go so soon made me
question why bother at all? In the face of so much struggle, so much of which
that we couldn’t resolve… Why bother facing anything at all? It didn’t make
sense.
Scrolling down Facebook, watching Youtube video after Youtube video… unfeeling,
uncaring. Questioning why continue at all? Until one day, I talked to someone
about it. My father. He came up and hugged me from behind, and just held me.
bother?” He’d sensed I was going through something. He didn’t know why. But he
did. A parent’s intuition maybe.
Everyone in this world will die someday.” An abrupt start to what I’d expected
would be an inspiring, or inappropriate joke, something frequently gushing from
his mouth to be sure. But he continued, “We can’t control that. What we can
control, is what we do in our lives. We focus on doing our responsibility, and
that’s all, as best as we can. And where we can, we leave this place a better
state than we found it in.”
is a fundamental truth of humanity.
of being an active member of a community, in the essential sense of the connection
that humans need to survive.
I’d always wanted to help people. It was just the right thing to do, it seemed. It’s why I’d wanted to do medicine. Cancer just cemented that. But I realised that it also is the best thing you can do, not just for others, but also yourself.
Because that feeling of putting a smile on someone’s face, or easing someone’s struggles… unlike things like fame, money, power, men or women – all those things we seem to desire most in life, that can never be taken away from you. That will never seem meaningless. That’s something you can always do.
And I want to share 1 unwaverable truth to all the doctors, medical staff, and regular people out there reading this…
No matter how dire things seem, no matter how much you feel like you’re just a cog in this machine which keeps churning out pain and death, no matter how much you feel hope, and powerless – YOU CAN, and DO, ALWAYS MAKE A DIFFERENCE.
No matter what the outcome.
Because what made my doctors special wasn’t the medical calls they made or their knowledge and prowess, what made my doctors REALLY special to me was the times they’d talk about my biking progress or my basketball before an appointment (that alone mitigated the 1 – 2 hour wait to see them)… the time one doctor walked alongside me and chatted on the way to a lung plural biopsy which I knew was gonna hurt. It was the time my doctor decided to write in to the medical entrance board and allow me to sit the exams that would allow me to become a med student. THAT’S WHAT MADE THEM SPECIAL… to ME.
I’ve sat down with men who were dying’s families and held their hands as they knew they were about to go, and been told by their family that that night we played snakes and ladders a few days before he passed was something he remembered on his deathbed itself. That the barbecue one friend had on father’s day, when a companion of mine in hospital had finally gotten gate-leave on Father’s day was the best barbecue and one of the best meals he’d had in his life.
But to those reading this, I also want you to know also that you don’t have to go this far to create change. Because the little things are Huge. They not only give fleeting happiness to your patients, your small gestures, and make you feel HUGELY cared for too as a patient… something that I realised I hadn’t felt when I had severe, suicidal depression for a year until I visited my old doctor, who’d treated me first (thank God I didn’t take that jump on that day.)… They also make you realise, at a doctor, that YOU ARE making a difference.That YOU DO matter… Those little acts of kindness reinvigorate you.
And if you take that opportunity to be the light in peoples’ darkest day, instead of going into work everyday thinking “Oh here we go, another 12 hour shift where I’m looking after people I can’t even listen to me, yet alone help or save”, “you’ll be thinking, “whose day can I make… whose pain can I ease… whose LIFE can I change?”
And that’s huge. It’s the difference between this being a job and a profession. It’s the difference between being run down or turning to alcohol or drugs to get by, and feeling fulfilled. It’s the difference between life and death.
So go out there and take every opportunity you can to do it. When you have a spare few minutes, take a few moments to see what allied health services around you can do to help improve quality of life for your patients and refer people to social workers to see how you can improve their lifestyles. They’ve made huge changes to my life, and so many others. It takes a median of 15 years for people to go see a pain clinic, for instance. Let’s fix that.
And if you still feel sometimes down despite it all, please, do get help. The biggest reasons doctors don’t seek help is fear for their career, or what their peers will think about them.
If that’s you, let me tell you this. I’m a man who used his mind to find a way of smiling, despite his cancer, 3 days after being told he’d had it at 17. I’m a man who’s ridden 200km 2 months after chemo for cancer charity. I’m a man one who’s running 2 social enterprises, one of which will save HUNDREDS OF THOUSANDS and BILLIONS in healthcare expenditure and most importantly… I’m man who found a way to smile after he’d been told he’d relapsed and that palliative care was a very good option in JUST 10 MINUTES…
But I still couldn’t outthink depression.
I still was miserable, despite my fighting against it and willing myself on, again and again. I still went into that deep dark place of wondering what’s my point in my mind when the pain I face struck.
If others think are thinking you’re weak… then they’d better have done more than me. Otherwise, whoever is or would, is someone who doesn’t understand something that should be basic knowledge. Someone judgemental and incapable of thinking outside the tiny little box that guides their life experience. Someone beneath your concern, someone who you wouldn’t want to befriend anyway.
Someone you shouldn’t worry about, or let get into your way to becoming the most content version of yourself – something you do deserve, no matter what depression makes you feel otherwise. I say this because one of the other biggest reasons we don’t get help is because we’re embarrassed.
Sometimes that person is yourself. Most of us are strong people. We power on. We’ve gotten through gruelling pre-med studies, then through medical schools and internship and everything that comes with the job, or in the struggle to get there. We can beat this. Or we can’t be one of those losers or sadsacks or whiners who suffers. We just get on with it. Scraping by, as some of us always have.
But getting help isn’t the “weak” option. You don’t get anything out of beating it. Why risk proving it to yourself, or put it off, or dismiss it as unnecessary, or just chinning up, and putting on a facade when you can get help to get you through it.
And I can tell you that when I got help, this all changed. Instead of walking in front of a train that day, I decided to walk across the street from the lab I worked in to see my old doctor, tired, cramping and feeling so alone. And thankfully, he was there. He just sat there, talked, and acted as any person would for another. He did what any doctor should do. He cared for me. As well as took care of me. He sent me to emergency, something you guys reading on mostly likely wouldn’t have to do, and I saw a psychiatrist. When I saw her, she said I wasn’t despondent, and didn’t need admitting, but would require therapy, for some time. When I asked about an SSRI (I’d noticed something was wrong for weeks), I remembered tbere was a drug I’d looked up for my unexplainable, untreatable cramping called duloxetine. I suggested it instead of the one she’d prescribed… and on day 2 of it… I not only lost this fog that was clouding my brain for a year every single day that I now know was depression, I also stopped feeling the pain. I’d felt as good as I had for years! Since before cancer. But it wasn’t just a drug that got me there, and got me to stay there.
It was talking to someone about it. My psychiatrist, he mainly does psychotherapy. Indeed, his goal is to minimise drugs (indeed, I’ve eliminated all of my psychiatric;neurological ones for that depression currently), and I recommend seeing someone who does too – maybe a psychologist, perhaps your nations’ doctor – doctor help line or mental health service (something I found out at that national doctors’ conference that we did for the first time). It seems confronting to do – open yourself up and admit things that you’ve never admitted before – to others or yourself – but the very things that make it seem confronting are the very reasons why it’s great.
What you say, can never leave his or her office. You’ll never see them in day to day life, or even have to see them again if you don’t want to. They are literally professionals at their jobs. And whatever you say to them, they legally can’t disclose to anyone! I encourage you to take that first step of reaching out to one, if you haven’t before, and think you may benefit.
And finally, I’d like to say thanks. You may not hear it a lot as doctors. It seems we patients are becoming less and less grateful over the years, but you guys really to matter to us. You see 20, 30, some of you, even 50 or 60 (in India, that’s common according to my Uncle), but we only see 1. It seems like a huge burden when you put it that way. But it’s also a huge opportunity. I hope what I’ve said convinces you to seize it with all your heart.
Nikhil
If you’d like to talk. I’m always here.
Suicide hotlines: 13 11 14 – Lifeline Australia. Add a +61 after your international dialing requirement and punch this number if you don’t have an alternative.
American: https://suicidepreventionlifeline.org
A 24/7 hotline where you can talk to another doctor anytime –
And I’d like to announce what I’m doing for the first time on this blog. I’ve started up a social enterprise that’ll, as said above, save hundreds of thousands and billions of dollars a year! Check it out at www.gettosleepeasy.org – here’s what it is.