So masks are great. We should be wearing them when we need to go out.<\/p>\n
<\/p>\n
But they don’t make you bulletproof.<\/p>\n
<\/p>\n
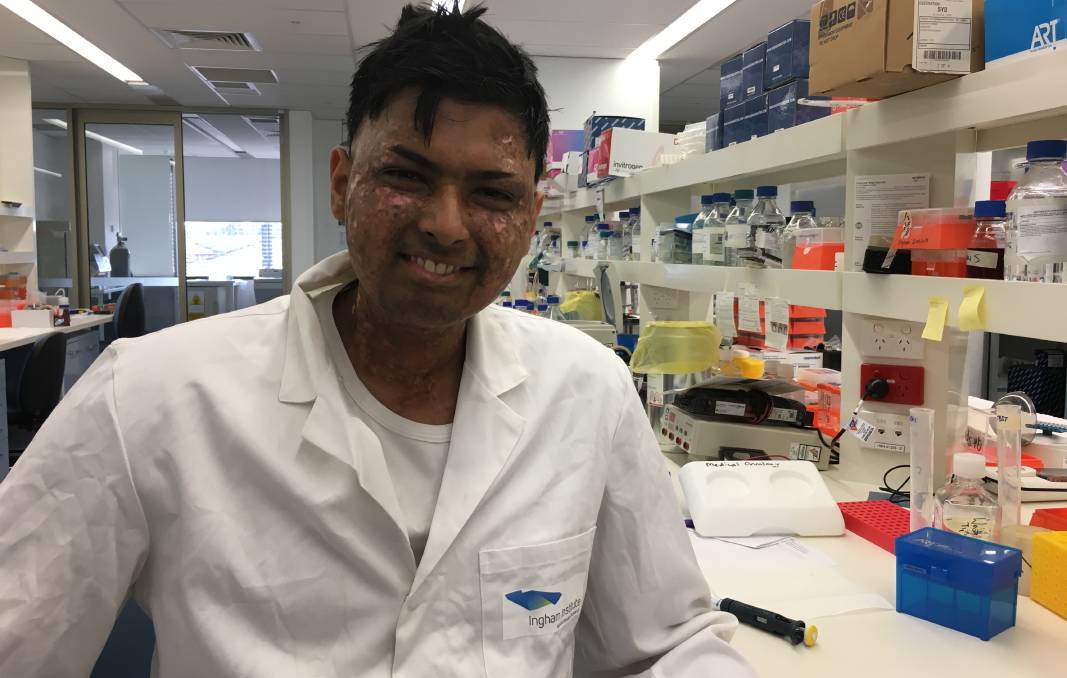
I\u2019m writing this because I\u2019ve seen and been talking to a couple of very high risk friends, one who’s actively getting cancer treatment, the other halfway around the world, going out with masks. When I asked one – a friend who is on chemo (I was shocked that he was going to a stranger’s birthday party while Melbourne’s lockdown was going strong) – he said that did so because he’s wearing a mask, and that he should be fine. He\u2019s either using a mask as a justification, or going out because of the mask.<\/p>\n
<\/p>\n
It’s nuanced. It’s not easy to communicate, because we do want people wearing masks when they go out. But for years, its been suggested that we shouldn’t be giving people a false sense of security with mask usage[1,2]. The WHO didn\u2019t make this suggestion out of the blue, as many on #MedTwitter suggest. Even studies modelling mask usage controlling the virus mention this[3].<\/p>\n

\nThere is evidence showing that this isn’t just conjecture too. This study used a location app to track individuals\u2019 habits in mask mandated areas vs non mask mandated one. Those in mask mandate regions spent 20-30 less minutes at home, and more time in commercial locations directly after the mandates! It could be contributing to spread if there aren’t further measures taken by cities [4]. To be fair, this is a preprint, but unless it’s fraudulent, or sample sizes are incredibly small, a sharp drop in household days after mask mandates were given is telling. Perhaps it\u2019s the mask mandates as opposed to the mask which got people to want to go out more. But that points to communication being an issue!<\/p>\n
On the other hand, there is a review which suggests that mask doesn’t increase the risk of people going out that went viral. But though the medical world latched onto this, the study only showed that mask usage didn’t reduce handwashing. It didn’t (because frankly, it hasn’t been studied until recently), find if mask usage increased distancing[5].<\/p>\n
<\/p>\n
I’m not saying that you shouldn’t wear a mask! The very opposite. Mask usage likely does reduce your risk of contracting a virus, and it IS definitively, through many studies, shown to reduce transmission if you happen to be ill in the community [7-9]!<\/p>\n
<\/p>\n
But we should be telling people to wear a mask – IF You need to go out.<\/h1>\n
<\/p>\n
ESPECIALLY to those at higher risk. As many as 50% of the population in developed nations have a risk factor that increases mortality risk with COVID-19. There are many dying in their 30s. Long term complications are still not known!<\/p>\n
<\/p>\n
If you’re at risk – Please, where possible, avoid going out if coronavirus is raging in your area. Listen to local health bodies and your doctors. That mask WILL reduce your risk most likely when you NEED to leave the home. And it can’t hurt you. But you shouldn’t be convinced that it will protect you. Even if you’re protesting a very good cause – if you or loved ones you interact with are at risk – I’d suggest you stay home.<\/p>\n
 <\/p>\n
<\/p>\n
<\/p>\n
<\/p>\n
The fact is – the WHO came out early on not recommending masks, as did many other nations, because the small studies that have been done on them show that in community settings – mask usage doesn’t reduce your risk of infection.<\/p>\n
This RCT showed that it didn’t reduce your risk of catching disease significantly in younger populations[6] This RCT showed difference either \u2013 though its primary aim was to look at household transmission reduction, it showed that influenza like illness (a primary way flus are tracked) contraction was similar in mask\/non masked groups [10]. They definitely DO reduce your risk of contracting illness, if they’re fitted n95s where users are trained in their use, as this review shows[7]. But that’s very different from community use.<\/p>\n
Though countries like China and Japan are pointed to as proof of masks working, a study of Japanese mask usage has actually shown that it\u2019s not masks, but rather the differing habits of mask\/non mask users, that lowers their risk of contracting viral illnesses. People who wear masks tend to go out less, and wash their hands more than non mask wearing counterparts[11]. A similar study of Hong Kong residents found similar results[12].<\/p>\n
<\/p>\n
But again, they definitely reduce your risk of transmitting disease to someone else, as I mentioned above[7-9]. And though statistically significant lowered rate of infection in these community studies wasn\u2019t reached – you need up to 10,000+ people to get surveys like this to have statistical power (though this was an RCT, 1000 people to track a whole populations\u2019 risk of flu may not be enough) \u2013 reductions in mask groups were seen.<\/p>\n
Various lab bench\/cough-simulating studies, like this one where outward particle emission was reduced by 90% on speaking[13], and common sense, we can tell that it will likely reduce your risk of contracting illness from droplets at the very least \u2013 even if it only stops you from touching your face as much[14]. But there are some studies disputing that masks even lower transmission with SARS-COV-2[15].<\/p>\n
<\/p>\n
That\u2019s why I emphasise, if you\u2019re at higher risk \u2013 your best course of action is to stay away from sick people in the first place!<\/p>\n
<\/p>\n
If you want to subscribe to an email list that’ll let you know if you can help scientists answer easy questions – check out CAroundYou.com\/ProveIt<\/a><\/p>\n I’m not gonna bother referencing properly as I’m not on my desktop which has EndNote, but should – I may later.<\/p>\n 1) https:\/\/www.bmj.com\/content\/369\/bmj.m2003<\/p>\n 2) Culture matters a lot when it comes to mask usage and its efficacy. Really interesting look into this;<\/p>\n https:\/\/www.ncbi.nlm.nih.gov\/pmc\/articles\/PMC4868614\/<\/p>\n 3) https:\/\/royalsocietypublishing.org\/doi\/10.1098\/rspa.2020.0376<\/p>\n 4) https:\/\/www.medrxiv.org\/content\/10.1101\/2020.05.23.20111302v2<\/p>\n 5) https:\/\/www.bmj.com\/content\/370\/bmj.m2913<\/p>\n 6) https:\/\/www.ncbi.nlm.nih.gov\/pmc\/articles\/PMC3266257\/<\/p>\n 7) https:\/\/www.ncbi.nlm.nih.gov\/pmc\/articles\/PMC5779801\/<\/a><\/p>\n 8) https:\/\/pubmed.ncbi.nlm.nih.gov\/19193267\/<\/a><\/p>\n 9) https:\/\/pubmed.ncbi.nlm.nih.gov\/18461182\/<\/a><\/p>\n 10) https:\/\/www.acpjournals.org\/doi\/full\/10.7326\/0003-4819-151-7-200910060-00142<\/p>\n 11) https:\/\/pubmed.ncbi.nlm.nih.gov\/23227885\/<\/p>\n 12) https:\/\/pubmed.ncbi.nlm.nih.gov\/16318726\/<\/a> – like Japanese study.<\/p>\n 13] https:\/\/www.nature.com\/articles\/s41598-020-72798-7<\/a><\/p>\n 14) https:\/\/www.ncbi.nlm.nih.gov\/pmc\/articles\/PMC7321045\/<\/a><\/p>\nReferences;<\/h4>\n