I wrote this up for a friend recently. And as some of you who follow me know, I’m writing a book about my experiences through cancer, and the science behind the mentality which kept me going. But I realised recently that I hadn’t written up what I wished I did have when I was suffering most from chronic pain… A step-by-step guide which showed HOW you could beat this back.
The thing is – when you have something like chronic pain… everyone around you has suggestions. Eeryone suddenly becomes an expert. When you’re already so drained, physically and emotionally, from the condition itself – being told about miracle cures and being sold things that ‘WILL CURE IT ALL’ is not only heartbreaking, when you find measure after measure fails, but also depressing, in and of itself.
So I’m telling you straight up – this isn’t a miracle cure. I still have issues dealing with the sleep and fatigue I get from this chronic pain/cramping/fibromyalgic-like condition that I have. I still do get frustrated by how it limits me, fatigue wise, at times (though I can ignore the fatigue as well, I know it’s healthy to respond to REAL signs it needs rest).
With this mental process, I still feel pain sometimes. But my suffering because of pain has decreased almost completely.
But the great thing about this is… It wasn’t even hard. It didn’t require an ounce or bravery/courage or willpower. It did take time. But to this day, I can, and do ignore pain as it comes on, automatically, 6 years on. Without effort, or an ounce of courage or “strength” that I frankly couldn’t muster back then. Almost no-one who’s faced real pain can.
I hope it helps you get to a point where you can ignore the pain, and reduce the depression pain brings too.
The Process. How To Ignore Chronic Pain.
It took a few weeks to get there. But key key to this is that I had a long term goal in mind – of becoming a person whose mind would automatically ignore the pain when it came on.
I knew I could do this because I was on duloxetine – an antidepressant – for a while 2 years ago, which helped me, despite it not actually stopping the cramps which were responsible for my pain. While I was on it… the pain still happened. But it didn’t affect me . This powerful evidence of me knowing it worked – of me being able to ignore pain – in the past, really helped get through my head that I could indeed accomplish this. That I COULD ignore chronic pain, which really helped me believe I could do it.
Here’s the thing though – YOU have proof of yourself ignoring pain too. Because all duloxetine is, is an antidepressant. It causes neurochemicals in your brain to make you feel happy, or happier than before.
YOU – when you’ve been happy, when you’re doing something fun, do the exact same thing. You HAVE ignored pain in the past. And that’s HUGE.
In the first few days (and it really only takes a few days to a week, max) of adapting this mindset, that belief, that KNOWLEDGE I had, and do beat back pain, is what motivated me to keep going through this process, which creates, and solidifies neural circuits in your brain, that help you ignore chronic pain. Automatically.
Reading about the science of chronic pain, and understanding it, only solidified that belief further. I looked at how greater connections between attentional centres and emotional ones, amongst others sensitizes us to, and enhances the impact of pain via maladaptive, or unnecessarrily bad neuroplasticity.
I also read about neuroplasticity in general (the science of habit formation in particular), and the effects of positive reinforcement (not ‘omg you’re the best!!!’ positive, but rather you Telling yourself when you’re right, to help affirm how you did something) on strengthening mesolimbic reward pathways. These mesolimbic pathways have numerous effects that makes a thought process or behaviour (and hence, easier to maintain) – from our amygdala (emotional centre), to the pre-frontal cortex (planning and attention centre), to our hippocampus (a vital part of memory).
But in the end – all you need to know is that when neurons Wire Together – they Fire Together. By firing off the same thought processes (which are ultimately a bunch of electrical signals) over and over – your neurons become more sensitive to being activated the same way. And they physically transform to have stronger connections. And as electricity goes down the path of least resistance, in time, this becomes the automatic way your brain deals with something!
By understanding everything I could about neuroplasticity, learning and motivation science, and combining my findings, I figured out how I could hack this process, through positive reinforcement (again NOT reaffirmations, but through constantly reminding yourself HOW you thought through something!)- so you could do it again.
Ultimately, this makes the journey to get to a stage where neuroplasticity would change my reaction to pain, easier. Below, I go into this process, step by step, in a manner that could help you out too! Here’s a video on it if you’re interested in the science. But really… underneath it all… it also just makes sense.
I talk more about this, and referencing hundreds of articles which helped me ‘hack my brain’ in my book – which is free! Just click there.
The 4 Steps to Make Ignoring Pain your Norm.
These steps I keep talking about are not only simple and replicable, but they make adapting this mindset, and making it your normal way of dealing with pain, easy too! What I do is I:
1) Take a step back and look at the pain I was facing – when it was worst, when it was best etc. I figured that out, and I wrote it all down.
2) I saw that I could, and did ignore pain when I was feeling happy, when I was on that antidepressant (it didn’t reduce the cramps themselves, but did help me ignore them). You don’t have to stop the pain at the source – you often can’t do that.
When you are able to attach less importance to a burst of pain and suffering though – you don’t feel it. I LATCH onto that.
3) I know now that I can, I do ignore pain sometimes… I saw that “As antidepressants caused me to ignore, and not be affected by pain, let’s focus on getting the same chemicals going on inside me to ensure I’m not affected by it!
By (a) Distracting myself! When you have chronic pain, your attentional centres in your frontal cortex grow visibly (we can see it in scans!) in size. Focusing on pain makes it worse. Do the opposite – distract yourself and focus on something else – and do this a few times in a row… and it starts becoming how you deal with things. and then
b) Focusing on something, or doing something that made me happy – like antidepressants do. That makes staying distracted easier. Do it enough times in a row – it becomes a habit.
I knew that process of making this your automatic, normal response, would take only a few weeks – as neuroplasticity causes LITERAL NEURAL CIRCUITS to form in that time.
In this case, of ignoring pain, It only takes 4 – 6 weeks to do this to a point where it lasts FOREVER.
But it only takes days to start not having to think, and consciously remind yourself to distract yourself, to start happing automatically.
By doing this – Almost mantra like – Instead of focusing on the pain once it occurred, I told myself “This Pain. All it is, is an aberrant, FAULTY signal that I shouldn’t be attaching significance to,” that “it would be over in seconds – minutes” that “getting annoyed by it, fretting over it happening again was only gonna make it worse (literally as remember – attention makes pain worse!). I told myself that “focusing on something else was more constructive – why not do that instead?”
and
4) I rewarded myself every time I ignored the pain.
I told myself it would take time. But I treated it as a long term goal I was working towards. If I allowed myself to be human – to crash, and acknowledge there would be times I’d be unable to ignore pain along the way, I’d be able to get back up when that did happen.
I’d remember that in the long run, if I managed to do this more often than not… I would become someone who could ignore pain automatically.
It wasn’t because I was brave… It wasn’t because I had raw ‘willpower…’ It’s literally basic biology. It was the only way things could go!
After a week, as I got better at distracting myself, and inducing happiness, I even started looking forward to cramps coming on as an opportunity to show myself I could do it! I’d addicted myself to getting better at doing this. I treated it like a game, that I was improving at. I did improve. I was winning.
In less than a month, my reward pathways kicked in and I didn’t have to keep reminding myself to ignore the pain, and talk to a friend, or put on a movie, or do anything again. I only had to think about Tom n Jerry, and I’d be able to smile inside, and change how I responded to the pain.
And the better I got at doing that, the easier it was to distract myself and feel proud that I could. It doesn’t hurt that when you give yourself a long term goal, you release exponentially more dopamine (our happy neurotransmitter), the closer you get to achieving it.
In 5-6 weeks, I didn’t have to tell myself any of this at all. I was automatically ignoring chronic pain when it struck. IT DIDN’T EVEN TAKE WILLPOWER – or me reminding myself of those ‘mantras’-cum-realisations I did in step 1 and 2. Neuroplasticity made this a habit. One I maintain to this day, 6 years later.
Maybe this could help some of you guys out too.
It isn’t perfect. When I cramp these days, I do still feel a jolt of pain, and it does still stop me from doing things as it physically takes a lot more effort to do things when you’ve got other issues like I do.
But I have been able to ignore the pain more often than not. Over 95% of the time.
My psychologist told me “you have to accept the pain”. But doing that was REALLY HARD – accepting that and saying “I may suffer like this all the time…” was impossible for me to just jump straight into. CBT and all that, I mean it could have helped, maybe… but again… that was hard to maintain.
It was the preparation of this mindset – the manipulation of my reward pathways and neuroplasticity – and the knowledge I could change how I deal with pain – that helped me stay on track.
The acknowledgement that it’d take time, and knowing I’d fail and feel crappy some days – but that in the long run, I’d get there – prepared me.
When failure did come, when I felt pain overcome me (I knew I inevitably would in my journey), I’d grit my teeth and bear it, but found myself focusing on the long run, and taking solace in that I would get there. I didn’t have to be this ‘brave, strong dude who had to ignore everything.’ By not having to be that guy, and by knowing how my brain worked, and that if I just walked myself through this more often than not, I didn’t just have faith that I could ignore pain. I KNEW IT.
But ultimately – the thing that helped me most was the realisation that this life can be very long. Why make my suffering worse by lingering on it? Why let it take anything more than me than it should?
That is what helped me persist with this and get to this stage I’m at now, where I do ignore pain, as an automatic response, when it comes on.
AND I KNOW YOU CAN DO THIS TOO.
I think it could possibly help some of you. I wrote this out for a friend, and realised I didn’t have a ‘lay-over’, something to help people as I kept working on that full sized book (don’t worry, it’s only going to be 30-40 pages). So I thought I’d share this with you guys too. Again – sign up to my email list (I only email people once a month or so, don’t worry), and you’ll know when that books’s finally out. I’m gonna try and make it free too!
I know how much is sucked being told “It’s all in your head” when I was really in the dumps because of all this, that’s why I don’t wanna kid you, and wanna let you know that it’s not perfect. You can ignore fatigue as well, I’ve found, but my recent health run-ins made me realise that ignoring legitimate signs your body is suffering (pain is not a good sign of this) is not exactly healthy.
But I hope my getting there can help some of you. Feel free to hit me up if you wanna talk it through – info at nikhilautar.com will give you a good chance of reaching me (I’m getting extraordinarily busy though – so this can’t be guaranteed). I’m also decently active on my Facebook page and have a startup – Bheem Health – I run (I got NSW Young Australian of the Year for this!) and Knia Maps – the Google Maps for Accessibility!) which I’m always working on.
Let me know your thoughts – good or bad (Please… ROAST ME if you hate this post. I wanna make sure what I’m saying helps the most people possible. I won’t mind at all if you completely hate this).
More about my pain condition –
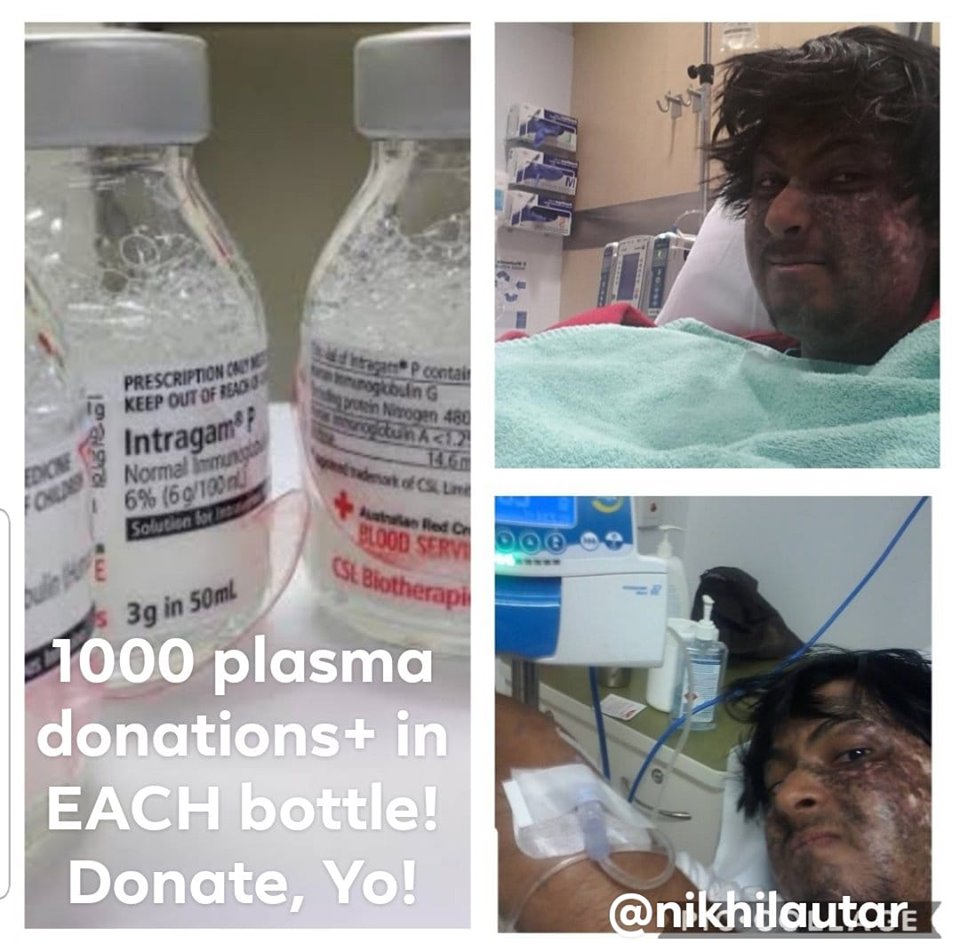
So I’m an ex leukaemia patient, current graft versus host disease sufferer and get chronic cramps. This is sort of common post transplant, but doctors aren’t too sure about what it is, how it happens, and have no clue about treating it in general. You can read more about my journey here.
Since writing this article, I’ve actually managed to fix my condition! My cramps affect me 95% less. I found a combo of drugs that work for it and am publishing it in medical journals.
I hope that this reminds you, that, for some of you… there is hope yet.