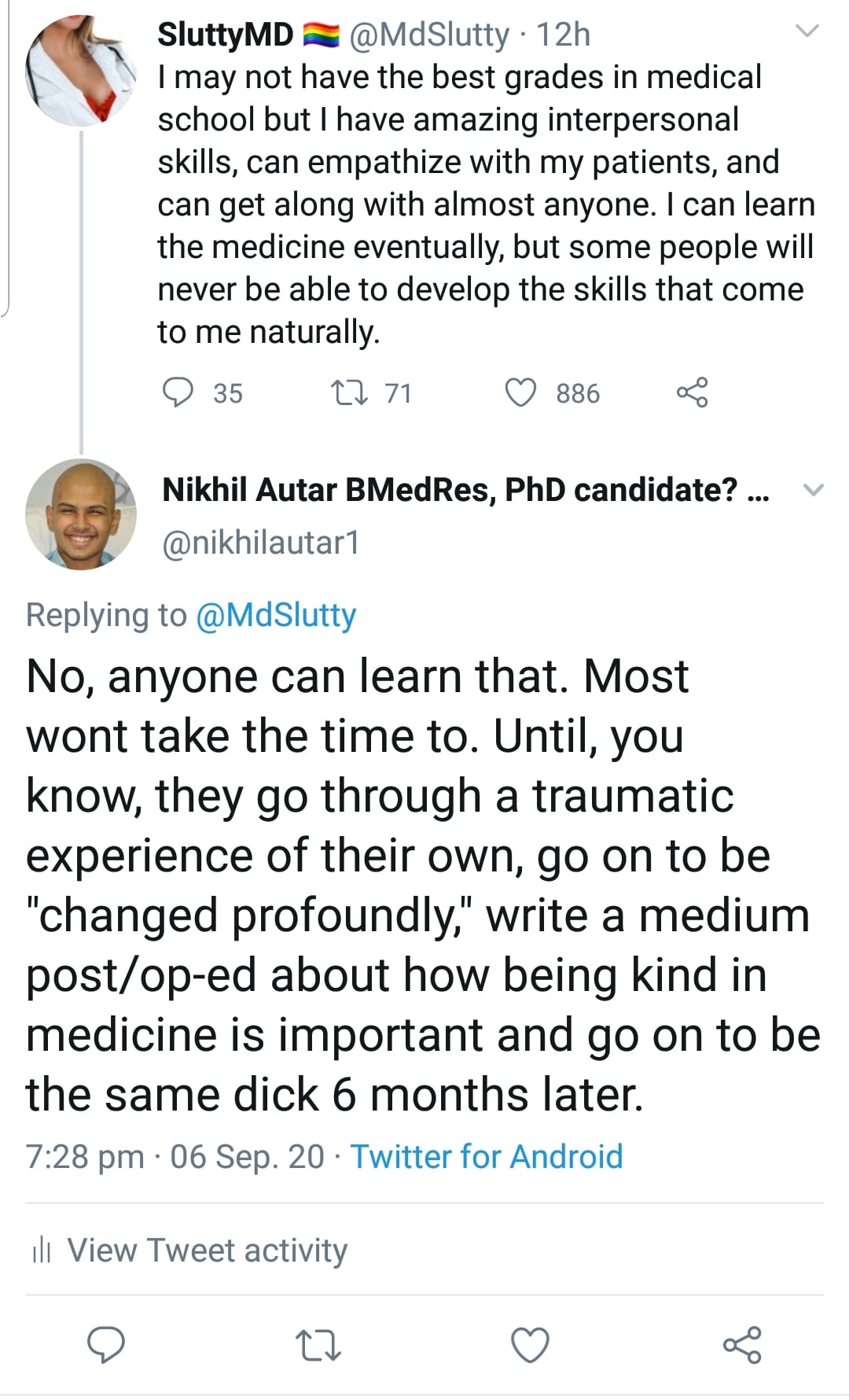
Recently, someone who follows this blog commented that they had no compassion for patients, and that this improved patient outcomes. It sounds heinous at first – god – someone like this in our profession? But he felt that there’s genuine merit to this idea. I know that at the very least, he’s a good nurse too. It was in response to a post I made on Twitter – below. He essentially asserted, and maintained after discussing with others, that he believes he delivers better care than others by not being compassionate, and focusing on evidence based care. It made me wonder, what is the actual evidence regarding the relationship between empathy/compassion and patient outcomes in healthcare.
It reminded me of a blog I read a while ago (I just can’t find it though!), of a doctor who said that in his department – emergency – they treated medicine like a job, as opposed to a service. And that this attitude led to lower levels of burnout.
He didn’t have any evidence to back that up. But it got me thinking – what is the evidence behind this? We know that burnout in doctors does lead to worse outcomes for patients. Should doctors and nurses distance themselves for the betterment of their patients?
So when he suggested the better option was his – apparently providing “more evidence based care in less time,” because he wasn’t spending time caring for patients, I dug into the evidence. This was my response;
“Yeah no, L. There is a dearth of evidence showing that patient centered care, which involves, heavily, taking care of people’s emotional needs as well as physical ones (for instance, ensuring physical comfort is maintained is important too), not only improves patient satisfaction, and reduces costs – but reduces mortality, and increases likeliness to come back and interact with healthcare too. Especially for those who are homeless (a population he prides himself on delivering better care to).
It doesn’t have to be a lot, or take heaps of time. There’s been recent support behind the 40 seconds of compassion model. But the “evidence” you say you put into your care, is just coldness. Other nurses and doctors ALWAYS practice with evidence too. They just do it better because they care as well. You think you’re a great nurse. You may be a good one, but you’ll never be a great one. Ultimately, the aim of healthcare isn’t to please or be liked by your peers or bosses. It’s to deliver good healthcare to people, and make sure people are happy as well. You can certainly do both by just doing your job, that is true. But you can’t confer the maximum benefit which leads to happiness and better outcomes.
A Ted Talk I’ll be watching tonight! The paper on this, I have read, and is linked below.
Having said that, there is an association of between burnout and poorer care and increased mortality. But distancing and detaching isn’t the fix – it’s actually associated with much worse rates of burnout. In some people though, they may have lower rates of burnout by detaching, you’re right. You may well be one of those cases. But you judging others who care as “wasting time,” when in fact, statistically, it’s shown YOU’RE wasting more time and resources, and contributing to worse outcomes by not giving as much of a damn as others, is 100% not fair.
I happen to agree that this cultural norm that seems to be propagated amongst physicians and nurses of ‘sacrificing for the good of the patient,” is probably taken too far by many. I know many doctors do suffer unnecessarily because of that, and some likely do burn out because of that. But the answer isn’t to detach – which creates EVEN MORE detachment, but rather to take time to care for yourself. If you’re happy and helthy yourself, you can give more of yourself, ultimately.
You do you – you may be one of the health professionals for whom not being compassionate may result in better care.
But don’t think you’re superior to others for it. According to the evidence, and likely from the patients you care for, you’re actually worse.
An excellent summary of the evidence showing patient centered, compassionate care results in better outcomes is in this paper – but I’ve linked several more for you to peruse as well. If you really care about evidence, have a look.
A report on the benefits of patient centered care – a model that advocates you involve patients in their care decisions, and that you provide both physical and emotional comfort to patients.
“Other benefits associated with patient-centred care include decreased mortality, decreased emergency department return visits, fewer medication errors, lower infection rates, higher functional status, improved clinical care, and improved liability claims experience.
In the care of patients with chronic conditions, studies indicate that patient-centred approaches can improve disease management; increase both patient and doctor satisfaction; increase patient engagement and task orientation; reduce anxiety; and improve quality of life.
Patient-centred care can also increase efficiency through fewer diagnostic tests and unnecessary referrals, and reduce hospital attendance rates. A patient-centred care approach has been linked to improvements in long-term outcomes in cardiac patients. Patient centred care is therefore regarded as an integral component of preventative care.
Increasing patient satisfaction through patient-centred approaches also increases employee satisfaction, and this, in turn, improves employee retention rates and the ability to continue practising patient-centred care.According to Charmel and Framton, the link between patient satisfaction and employee satisfaction is reflected in the fundamental philosophy of patientcentred care: the importance of staff feeling cared for themselves, so they can best care for their patients.”
https://www.safetyandquality.gov.au/sites/default/files/migrated/PCCC-DiscussPaper.pdf
More papers showing the benefits of compassion are linked below – including the largest systematic review on the topic. But I also believe, as you may have seen from the original Tweet above, that compassion and caring for patients isn’t an inherent trait that can’t be taught.
I believe it can and should be taught and mandated. Med school, or nursing school for that matter, is the best time to do this.

Me in my first clinic day of second year medicine!
“I was super shy and awkward in my first year of med school. A mixture
Reduced mortlaity even in myocardial infarction when more compassionate care was received – https://pubmed.ncbi.nlm.nih.gov/20662947/
Lowered pain, reduced anxiety, and faster healing, as well as higher likelihood of following care plans: https://www.novanthealth.org/healthy-headlines/the-healing-touch
https://pubmed.ncbi.nlm.nih.gov/15907021/
Just 40s of compassion resulted in better patient satisfaction.
https://pubmed.ncbi.nlm.nih.gov/10458256/
The largest systematic review found that burnout was negatively correlated to empathy. There are some studies which concluded the opposite, but they weren’t as high quality, and were in the vast minority.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5534210/
Burnout only decreases mildly with small amounts of detachment, but increases significantly when you detach more.
https://www.researchgate.net/publication/339402091_The_role_of_psychological_detachment_in_burnout_and_depression_A_longitudinal_study_of_Malaysian_workers_Burnout_and_Depression
In most studies – detachment is actually A MEASURE of burnout levels; https://www.researchgate.net/publication/260873755_Exhaustion_and_Lack_of_Psychological_Detachment_From_Work_During_Off-Job_Time_Moderator_Effects_of_Time_Pressure_and_Leisure_Experiences
It’s not compassion, but harder working conditions that’s related to burnout.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3662129/